Lifting the fog
Dr. Daniela Bota of UCI’s Comprehensive Brain Tumor Program is determined to find ways for cancer patients to avoid “chemo brain.”

After receiving her medical degree in her homeland of Romania, Dr. Daniela Bota came to the U.S. to earn a doctorate in molecular biology to better understand why people develop neurodegenerative diseases such as Alzheimer’s.
Eventually, Bota changed her focus to treating brain cancer, but her background in dementia is helping her identify ways to keep cancer patients from experiencing problems with concentration, thinking and memory after chemotherapy treatments.
This foglike phenomenon called “chemo brain” can be debilitating, not only for people with brain tumors but for those undergoing chemotherapy for other forms of cancer, she notes.
“We’re just beginning to understand the causes of chemo brain,” says Bota, an assistant professor of neurology at UC Irvine. “Doctors used to think the cognitive effects of chemotherapy were psychological, a form of depression. But we’re finding a biological basis.”
She and Dr. Mark Linskey, co-directors of UCI’s Comprehensive Brain Tumor Program, have discovered that certain chemotherapeutic agents destroy the stem cells in the brain that would have become neurons for creating and storing memories.
Both healthy tissue and cancerous tumors have their own versions of stem cells, the precursors that give rise to a variety of organs and other structures. But tumor stem cells grow chaotically and engender cancer cell proliferation.
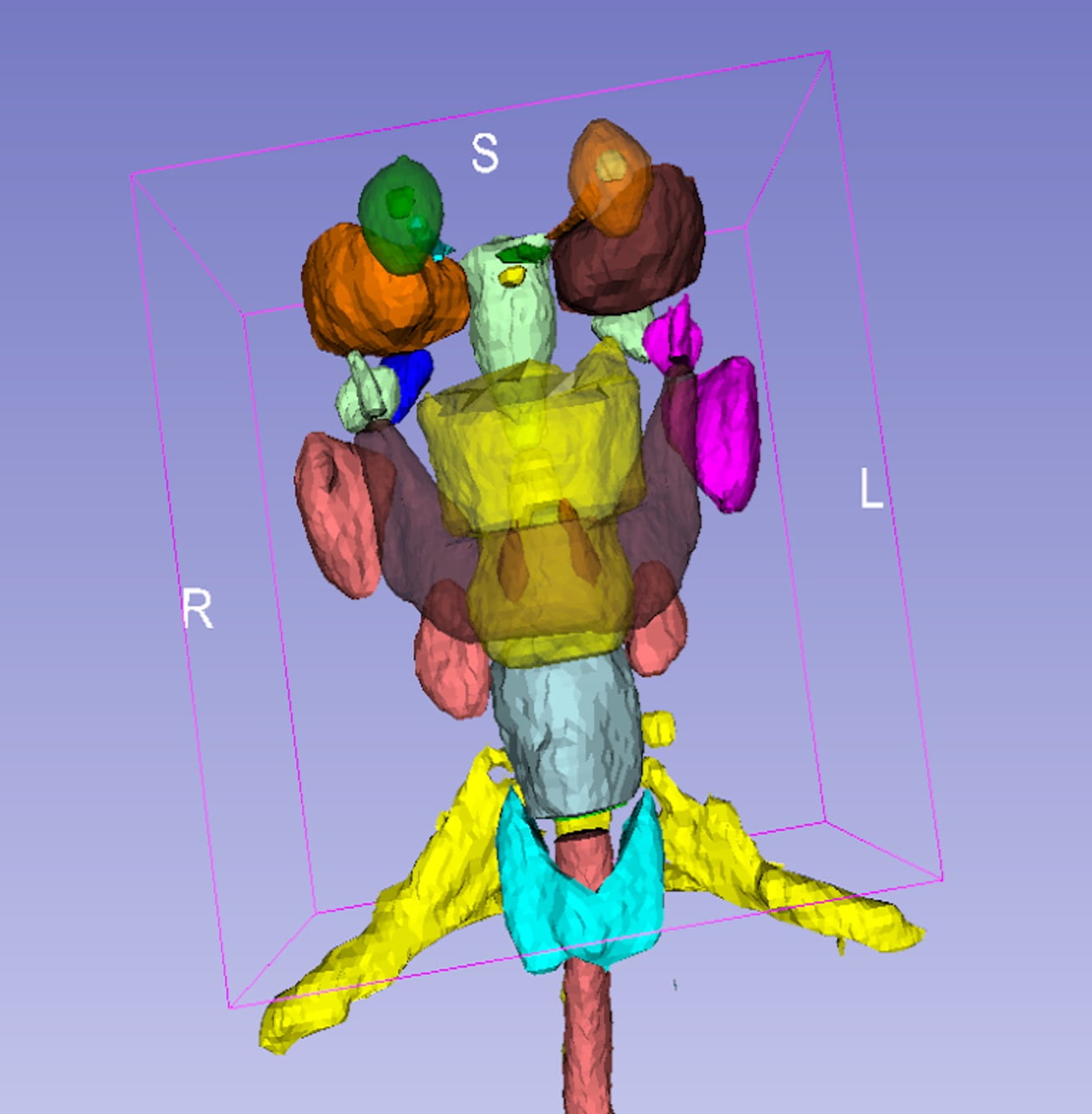
In laboratory studies on healthy brain stem cells and those that cause gliomas, or brain cancer, Bota and Linskey found that two widely used chemotherapies profoundly damaged healthy neural stem cells but had little effect on brain tumor stem cells. Two newer chemotherapy drugs they tested that specifically target tumor cell proteins, however, caused little or no harm to neural stem cells while wiping out the tumor’s stem cells.
The results — published earlier this year in Neurology — are causing a stir in the neurology and oncology communities and, if confirmed in clinical trials, point to the use of less-toxic chemotherapies in future cancer patients.
Children — who have as high as an 80 percent survival rate after chemotherapy for brain cancer — could be the biggest beneficiaries of all.
“The cognitive deficits these children might face can lower their quality of life and make it difficult to get on with their young lives,” Bota says. “Too often, what you see when the tumor is in remission is a patient with dementia.”
She came to UCI in 2007 and joined Linskey, a highly regarded neurosurgeon, in founding the Comprehensive Brain Tumor Program under the auspices of the Chao Family Comprehensive Cancer Center. It’s the only program of its kind in Orange County that offers clinical trials of breakthrough treatments for brain cancer.
As one of only about 300 neuro-oncologists in the country, Bota brings a distinctive perspective to fighting brain cancer. By combining the disciplines of neurology and oncology, she can evaluate and guide the comprehensive care of brain tumor patients. For instance, she’s able to assist those with seizures or cognitive difficulties while using the optimum combination of chemotherapy and radiation to attack their tumors.
“It’s rewarding to work with people who might not have any hope at first but then go on to enjoy things like a child’s graduation or the birth of grandchildren or other meaningful events they didn’t expect to see,” Bota says. “A lot of discoveries are being made in neurology and oncology involving brain tumors. We’re in an exciting time.”