Saving Mother and Child
Multidisciplinary teams of UCI oncologists and maternal-fetal specialists utilize scientific advances to treat patients with high-risk pregnancies
Five-year-old Emlee jumps high, runs fast and likes to pirouette around the living room in her white ballet slippers.
Her mom, Karalayne Maglinte, calls her a miracle. Indeed, Emlee is the embodiment of the word: She’s one of the reasons Maglinte is alive today. Another reason: High-risk pregnancy physicians and cancer specialists at UCI Health were able to help the Fontana woman when no one else could.
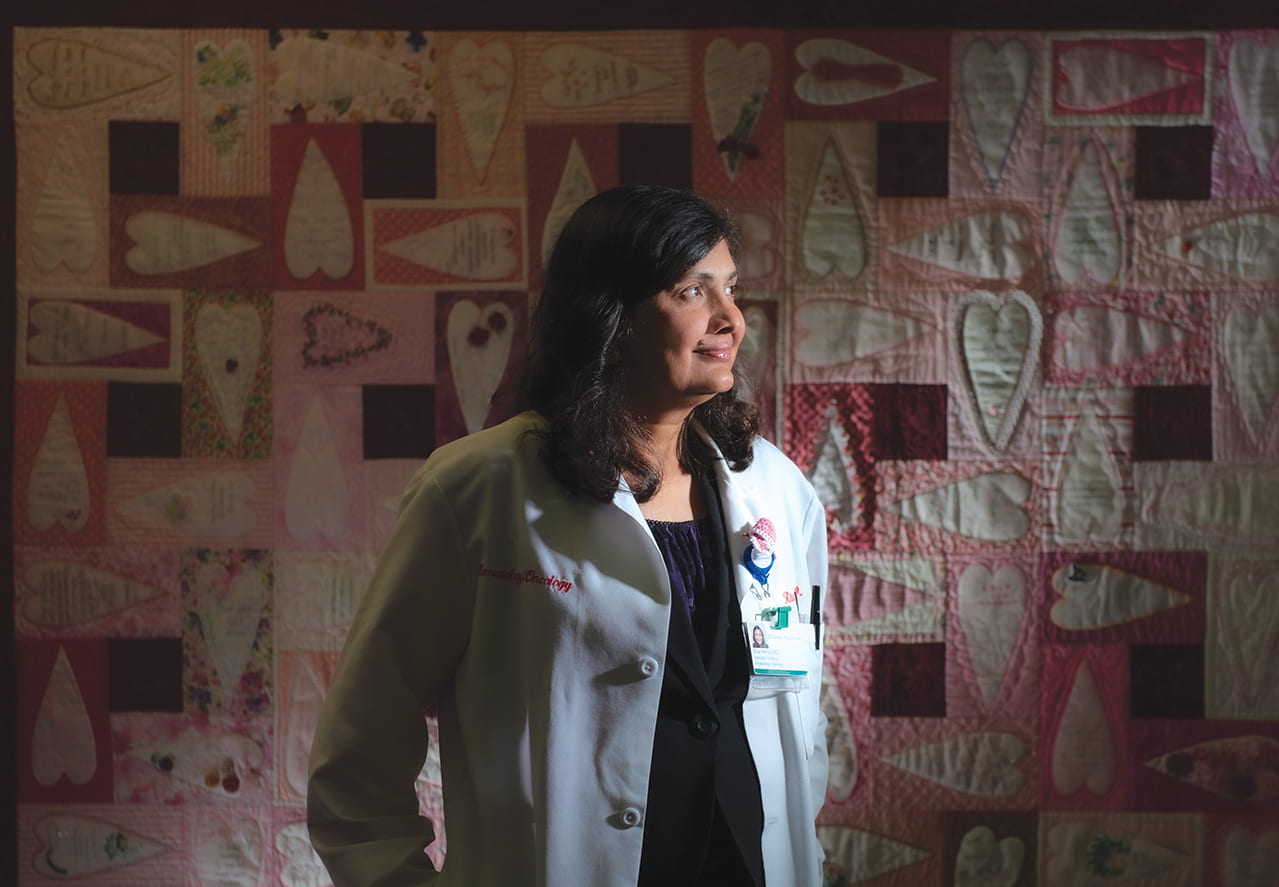
Cancer during pregnancy is a rare event, occurring approximately once per 1,000 pregnancies annually, according to the National Institutes of Health’s World Journal of Oncology. Fortunately, “we have plenty of experience treating patients who need a multidisciplinary approach,” says Dr. Rita Mehta, a UCI Health oncologist.
Mehta has cared for several pregnant women with cancer, including Michelle Clark-Salib, who was just 28 when diagnosed with breast cancer. Her son Caleb is now 7, and Clark-Salib is cancer-free.
But the situation was touch-and-go for a long time, just as it was for Karalayne and Emlee Maglinte. Their poignant story began to unfold in 2013 when Maglinte was 15 weeks pregnant. She was 36 years old and had two boys at home: Ian, 6, and Isaac, 18 months.
“Because I was pregnant, I was much more aware of my body’s cues that something wasn’t right, and I was quicker to react than I might have been otherwise,” Maglinte says.
“My hands and feet were itchy,” she says, “so itchy I wanted to tear them off.” She consulted “Dr. Google” and read that it might be a liver issue.
“At first I thought perhaps it was because I was pregnant with a girl, and the other two were boys,” Maglinte recalls. “But it got so intense that I began to worry. I didn’t want to endanger her.” The itchiness began on a Friday. By Monday, she was convinced she needed to call her doctor.
A Challenging Diagnosis
An arduous round of tests, physician appointments and hospitalizations ensued as several Inland Empire doctors tried unsuccessfully to diagnose and treat Maglinte. In addition to the itchiness, she developed jaundice. After four days at a community hospital, she was taken by ambulance in the middle of the night to UCI Douglas Hospital, in Orange.
A team quickly assembled, including high-risk maternal-fetal expert Dr. Julianne Toohey, gastrointestinal endoscopy specialist Dr. John Lee, and pancreatic cancer surgeons Dr. Aram Demirjian and Dr. David Imagawa.
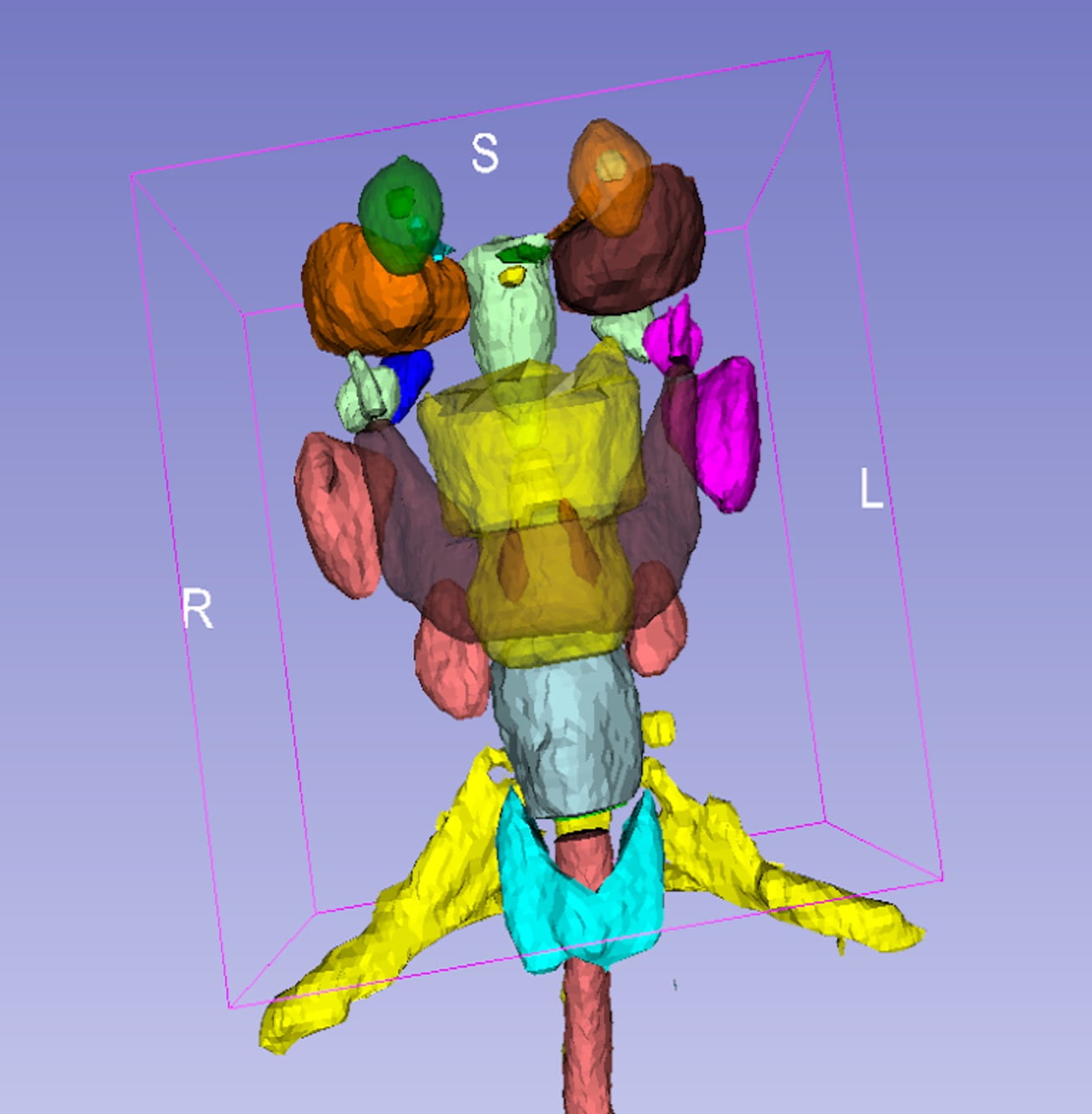
Lee – an authority in diseases of the liver, pancreas, bile ducts and gallbladder – examined Maglinte using endoscopic ultrasound. His findings led to a biopsy of her pancreas. He also implanted a bile duct stent to alleviate her jaundice. Although complex, each procedure was minimally invasive and safe for the baby.
But the diagnosis was daunting: Maglinte had an aggressive form of pancreatic cancer. “It’s strange that she would have had cancer at that age,” Lee notes. Statistically, almost all pancreatic cancer patients are older than 45, with the average age at the time of diagnosis being 70. Maglinte was only about half that.
She was devastated. “I kept walking around the halls of the maternity ward saying: ‘How the heck did I get here? This is crazy.’”
There weren’t many options. Early delivery “meant the baby would not have survived, as I was only 19 weeks pregnant,” Maglinte explains.
But she also had two children at home to consider. She and her husband, Dennis, discussed it. “He said it was my choice,” Maglinte relates. “I wanted to fight for her, but I also needed to fight for myself.”
The physicians worked together to save both mother and child. “Taking care of a high-risk patient with cancer involves careful communication with the whole team and, of course, the patient,” Toohey says. “Karalayne was very involved in decision-making.”
A week after the diagnosis, Demirjian operated, performing a seven-hour Whipple procedure, or pancreaticoduodenectomy, to remove the tumor. But Maglinte didn’t have chemotherapy, which would have jeopardized Emlee’s survival.
“We watched the baby’s growth and ended up with a planned delivery at 39 weeks,” Toohey recalls. “This is rather unusual with cancer patients – we usually deliver several weeks earlier in order for chemo or other treatment to begin as soon as possible.”
Happily, 7-pound, 1-ounce Emlee was born without complications. Her mom says she’s a “little lifesaver” because only 20 percent of pancreatic cancers are diagnosed early, mainly because symptoms – abdominal or mid-back pain, jaundice, weight loss and indigestion – can overlap with those of other conditions. “Without Emlee, I probably wouldn’t have reacted to my symptoms the way I did,” Maglinte says.
She and Emlee received the kind of advanced care that’s usually only available at an academic medical center like UCI.
Applying the Research
Oncologist Mehta, who joined the faculty in 2001 as a clinical professor of medicine, lauds the university, saying, “One of the great things is that not only can you do research here, but you can apply what you learn from that research to treat high-risk pregnancies with cutting-edge techniques. That’s not possible in a community hospital setting.”
That distinction was as important to Michelle Clark-Salib as it was to Maglinte. In 2012, at age 28, she was diagnosed with an aggressive 8-centimeter breast tumor. After undergoing nearly three months of chemotherapy with a community oncologist in Riverside, Clark-Salib found out that she was 23 weeks pregnant with her son Caleb.
The North Fontana woman consulted with an obstetrician, who discovered that her amniotic sac contained almost no fluid, a side effect of one of her chemo drugs that posed a serious threat to the developing fetus. The doctor sent Clark-Salib to the high-risk maternalfetal physicians at UCI Health, where he had trained as a resident.
Mehta, an international expert in metastatic breast cancer, eventually took over the case. “Michelle is an amazing young woman,” Mehta says. “She was at a very critical stage when she came to us but wanted to save her baby’s life and her own life. Abortion wasn’t an option for her.”
The drug that was causing the amniotic fluid problem was discontinued, and Mehta devised a modified cancer treatment plan that avoided the more toxic drug Herceptin until the infant arrived.
“As soon as the baby was delivered, we put her back on a chemotherapy regimen, and her cancer went into complete remission,” Mehta recalls. Caleb was born healthy at 37 weeks’ gestation.
“Survival rates are so much improved since I began working in oncology. Sometimes the steps are small; sometimes they’re bigger. But overall, each step adds to the next, and rates keep improving.”
Promising Scientific Advances
Mehta finds this an exciting time in her field: “Survival rates are so much improved since I began working in oncology. Sometimes the steps are small; sometimes they’re bigger. But overall, each step adds to the next, and rates keep improving.”
Over the last 15 years, her research has led to many advances in treating the most aggressive breast cancers. In a groundbreaking study published in 2012, Mehta showed that a combination of the drugs anastrozole and fulvestrant was superior in controlling cancer and improving patient survival to anastrozole alone or anastrozole followed by fulvestrant in treating hormone receptor-positive metastatic breast cancer in postmenopausal women. A long-term update of the study, published in March 2019 in The New England Journal of Medicine, confirmed the increase in five-year survival rates for advanced breast cancer patients.
Mehta was also one of the first to use chemotherapy combined with Herceptin on women with breast cancer before surgery – rather than only after – to help shrink tumors.
Now, more than seven years after Caleb’s birth, Clark-Salib remains cancer-free. And Maglinte has been cancer-free for more than six years.
“I don’t know what I would have done without UCI,” Maglinte says. “We were at the right place at the right time with the right teams. Everything just fell into line. Everyone we needed to be there was there.”