Making chemotherapy safer, more effective
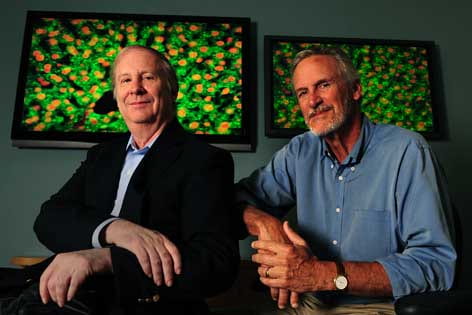
UCI researchers Kenneth Longmuir and Richard Robertson have developed a more precise approach to delivery of chemotherapy drugs.
Chemotherapy is one of the most effective ways to fight cancer, but the toxic medicine can cause collateral damage to healthy tissue.
UC Irvine’s Kenneth Longmuir, physiology & biophysics associate professor, and Richard Robertson, anatomy & neurobiology professor, believe they have developed a way for these drugs to reach specific tumors with increased precision, thereby limiting side effects.
In a study appearing online in the International Journal of Pharmaceutics, the researchers show that doxorubicin — commonly used to treat a number of cancers — can be directed almost entirely to a particular spot in the body with virtually no spread to other organs.
“Although doxorubicin is a potent anti-cancer agent, its usefulness is compromised by its serious side effects on normal tissue,” Longmuir says. “When administered in a chemotherapeutic regimen, the drug distributes widely in the body, including the heart, rather than just in tumor regions. This chance of heart damage restricts the amount of doxorubicin that a patient can receive.”
He notes that less than a quarter — and in many cases less than 10 percent — of the medicine typically reaches its target. The remainder is dispersed throughout normal organs, resulting in considerable toxicity.
To overcome this, the researchers focused on the fact that all tissue, even a tumor, is surrounded by a dense area of sugar-containing molecules called polysaccharides. The chemical composition of these polysaccharides differs for each type of tissue.
“We knew that if we could find a molecular guide to a specific polysaccharide coating, we could create a highly targeted drug delivery system,” Robertson says. “Fortunately, such a guide exists in the malaria microorganism Plasmodium.”
Plasmodium has the exceptional ability to only recognize the liver’s polysaccharide coating. So Robertson and Longmuir isolated the protein that allows Plasmodium to do this and built a doxorubicin delivery system around it.
They inserted the drug into fatty, tubelike structures called liposomes that are staples of nanomedicine. Then they bonded Plasmodium’s targeting protein to these liposome packages, in essence “addressing” them to the liver.
In tests on mice, the research team demonstrated that doxorubicin was conveyed to the liver, and away from the heart, with a specificity rate of more than 99 percent.
The next step is to try the drug transport system in several experimental cancer models, Longmuir says. He and Robertson are developing new liposome packages with targeting proteins that only recognize the unique polysaccharide features of tumors.
“By rapidly and accurately delivering chemotherapeutic agents to tumor regions, treatments can become safer and more effective,” Longmuir says. “This promising approach opens up a new avenue to helping people survive cancer.”