Compassion. Expertise. Trust.
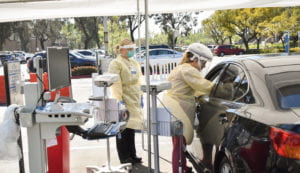
Susanne Phillips and seven nurse practitioners working at drive-thru COVID-19 testing centers embody theme of National Nurses Week

The man in his 20s had a look of dread in his eyes as he pulled up to the drive-thru COVID-19 testing center in Orange. His mother, sick with symptoms of the disease caused by SARS-CoV-2, was in the passenger seat.
“How long has she been sick?” asked Susanne Phillips, DNP, a clinical professor and associate dean of clinical affairs in the Sue and Bill Gross School of Nursing.
“About two weeks,” said the young man, translating for his Spanish-speaking mother, who is in her late 40s.
Phillips, a 27-year nursing veteran who in mid-March helped lead efforts to get Orange County’s first drive-thru screening site open next to the UCI Health Manchester Pavilion, began asking about the woman’s symptoms when her son interrupted her.
“If she has [COVID-19],” he asked, “is it a death sentence?”
“You could just see the look on his face,” Phillips recalls.
With National Nurses Week continuing through Florence Nightingale’s 200th birthday on Tuesday, May 12, nurses like Phillips are in the spotlight during an ongoing pandemic that has put them on the front lines.
“Compassion, Expertise, Trust.”
Dr. Steve Goldstein, vice chancellor of health affairs at UCI, wrote in a message to troops last week that this theme of National Nurses Week is an excellent three-word description of what nurses bring to each patient.
Phillips, seven nurse practitioners, two licensed vocational nurses and two medical assistants who staff the Manchester drive-thru test center, as well as a second location at the Gottschalk Medical Plaza on the UCI campus, strive to embody that theme.
“When [motorists] come through, many are anxious and nervous. Some of them have seen [in the media] really scary images of people being swabbed, and they’re afraid of the process,” Phillips says. “Being nurses, it’s not hard to talk somebody through this process and really calm their nerves. We provide them that human touch to show them we’re not just an assembly line of people swabbing noses – that on the other end of the swabs are caring humans.”
Eight weeks and counting
Taking a break to discuss her job between follow-up calls to patients and an online video conferencing chat she and her husband had with their two adult children who live on their own, Phillips said she’s worked every day the last eight weeks. But she wasn’t complaining.
“This is one of the most fulfilling projects I’ve ever worked on,” Phillips says. “We come into this profession knowing that there are going to be days when we’ll be caring for people and things seem very routine. And we know there’ll be times in our careers when we really have to step up.”
“You have to look at your own fears,” she adds. “But it’s the bigger picture that draws us toward the crisis and not away from it. We have our fears and our anxieties, but we know it’s important, and we step up.”
Phillips didn’t hesitate to raise her hand when, in mid-March, UCI Health leadership put out the word that the hospital needed help with the burgeoning demand for coronavirus testing.
“When the opportunity came to help the medical center, we jumped on it,” she says. “I knew our nurse faculty needed to be highly engaged in this COVID response.”
Phillips reached out to UCI Health Chief Nursing Officer Pat Patton to ask what he needed from them. He connected Phillips with Erwin Altamira, senior director of ambulatory care administration, who suggested that nurses could help with testing.
That discussion took place Friday, March 13.
Working with hospital leadership from ambulatory care administration, epidemiology & infection prevention, information technology, pathology & laboratory services, environmental health & safety and public safety, Phillips and her team had everything in place on Monday, March 16.
On March 17, the Manchester drive-thru test center began seeing patients by appointment. The Gottschalk location opened March 20.
As of Sunday, May 10, both drive-thru centers combined have tested hundreds of patients. (There is a third testing site at UCI Health Family Health Center in Santa Ana.)
Phillips coordinates both drive-up testing centers, which in the last week and a half have seen a dramatic increase in patients because of the resumption of elective surgeries and procedures. UCI Health patients scheduled for surgery or an invasive procedure are required to be screened for COVID-19.
Phillips is at the Manchester test site almost all the time.
On the weekends, from her home in Rancho Santa Margarita, she makes follow-up calls to inform patients of their test results, which notifying others through their electronic medical record.
Within a few weeks of testing, UCI Health began processing the COVID-19 tests in its own laboratory, shortening the time to result to approximately 24 hours. When the Manchester drive-thru center opened, results took between seven and 10 days because, at the time, UCI Health was using outside laboratories to process the tests.
“If a person tests positive,” Phillips explains, “the nurse practitioner who performed the test calls the patient no matter what day of the week it is. And we don’t just tell them they are positive for COVID-19 and leave them to figure out their own follow up. We go over the items we talked about when they were in the car – the need for strict isolation and masking, and making sure they have a room that they can stay in by themselves. We also ensure they have a healthcare provider to follow up with if they do not have a primary care provider.
“And even if their test is negative,” she adds, “if they don’t have a healthcare provider, we provide them with a number to call where they can make an appointment to be seen for further care.”
Phillips says many of the drive-thru patients she’s seen aren’t living in quarters large enough to practice safe social distancing.
“I’ve had a patient, a first responder, who was living in a two-bedroom house of eight people,” she says.
Phillips also recalls a family of seven. The father tested negative for COVID-19, the mother positive, and one of the children was hospitalized with the disease. The father was able to stay with his sick child at the hospital, while his wife – who was also very sick but didn’t require hospitalization – cared for their other four young children.
“It’s not like you have a cold, and [as a parent] you just make it work,” Phillips says. “These people [with COVID-19] are sick and need to rest.”
Phillips was able to put her assigned primary care provider, a nurse practitioner, in touch with the woman. That nurse then got a social worker involved.
“That’s the personal touch that we’re able to provide, and I’m really proud of it,” Phillips says.
Down time
In addition to working the Manchester drive-thru test center, Phillips has faculty responsibilities in the Sue and Bill Gross School of Nursing.
Her husband, Rob, a software engineer for the Automobile Club of Southern California who is working out of his home, will have dinner waiting for her after a long day of testing.
To unwind, Phillips will play with the couple’s two dogs, Jack and Lola, who are Maltipoos, a cross between a Maltese and poodle.
With spring in full bloom, Phillips has been getting some exercise and clearing her mind working in her backyard rose garden.
“I was just way too busy – literally, I wasn’t stopping and smelling the roses. They just existed, but I didn’t pay any attention. But my roses are special, and now I’m giving them a little bit of extra attention.”
Reassurance
The scared son who asked Phillips if COVID-19 was a death sentence for his mother was reassured by her answer.
“No,” she said to him. “Being positive doesn’t mean that. But I don’t really know how long she’s been ill to determine where in the course of illness she is. If she gets to a point where she cannot finish sentences without taking a breath in between words or in between a few words, I want you to call 911 and take her to the emergency room.”
The woman did test positive and was hospitalized, but Phillips doesn’t know her fate due to patient privacy laws.
She was happy to give the woman’s son some reassurance that day.
“At the end of the day,” she says, “everybody who comes to be tested or everybody who’s been impacted by this disease, whether or not they have money, everyone is human and deserves a human touch.”