Better than biopsies
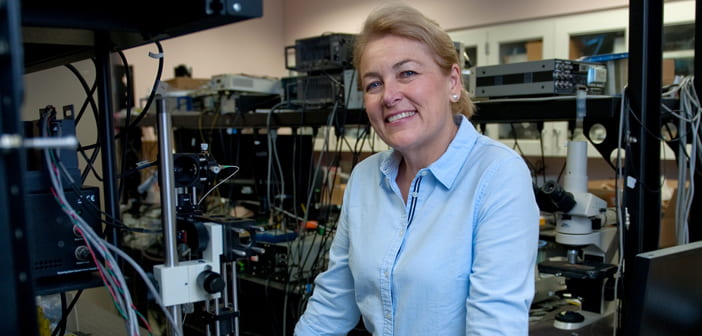
UCI’s Dr. Petra Wilder-Smith has pioneered the use of laser technology to noninvasively detect and treat oral cancers
Ever since her student days in the dental clinic at Guy’s Hospital in London, Dr. Petra Wilder-Smith has been looking for ways to do things differently.
At the time, regular biopsies were standard practice to monitor precancerous mouth lesions before they possibly metastasized. But in a majority of cases, the patients did not return after the first biopsy. It was just too painful.
“I knew there had to be a better way,” Wilder-Smith says.
She saw the light, so to speak, with the emerging use of lasers for medical purposes. So after gaining her dental surgery license in 1983, Wilder-Smith enrolled at Aachen University in Germany – a leading technological institute in Europe – to earn a doctorate in the applications of light and optics in oral diagnosis.
“I thought that this would be the better way,” she says. “And I was right.”
In 1992, Wilder-Smith joined UCI’s Beckman Laser Institute & Medical Clinic, where she’s now director of the dental program and a professor-in-residence. Over the past two decades, she has developed innovative techniques that utilize some of the world’s most sophisticated lasers to noninvasively probe into mouth lesions to determine the growth of cancerous cells and eradicate them.
“Petra is widely recognized for her visionary leadership in the pioneering use of optics and photonics technologies for improving oral health,” says Bruce Tromberg, director of the Beckman Laser Institute. “She has a special combination of abilities as a compassionate clinician with a unique understanding of patient needs, particularly in medically underserved communities.”
To advance better methods of tracking and treating oral cancers, Wilder-Smith collaborates with scientists and oncologists at the City of Hope, Cedars-Sinai, UCLA, USC and the University of Pennsylvania; and she has received consistent research funding from the National Institutes of Health, various groups in the U.S. Department of Defense and oral care companies.
“Dr. Wilder-Smith is a world leader in the field of optics for oral cancer,” says Dr. M.A. Kuriakose, chief of head and neck oncology at the Mazumdar-Shaw Cancer Center in Bangalore, India.
This work on diagnostics and early treatment is especially important for oral cancers, which are caused by a variety of factors, such as tobacco and alcohol use, HPV infections, poor diets and the chewing of betel quid, which is common in many parts of Asia. While the survival rates for stage 1 and 2 cancers are over 80 percent, those for stage 3 and 4 cancers are less than 40 percent. And according to Kuriakose, more than 70 percent of oral cancer patients first see a doctor at the latter two stages.
In low-resource nations like India, which has the planet’s highest burden of oral cancer, the situation is more acute, primarily due to a lack of awareness and – for the poor – access to specialized care. There are some 80,000 new cases of oral cancer annually in the country, and data from the Million Death Study shows that oral cavity cancer accounts for 35 percent of all cancer deaths among Indian men.
That’s why Wilder-Smith and Kuriakose have partnered to develop and test a low-cost, portable screening device that field-workers in India can use to detect possible oral cancer. The technology would enable these people – many of whom rarely see dentists – to receive early-stage care and dramatically improve their outcomes.
A solar-powered device slightly larger than a shoebox, it can take laser images of oral lesions that will be sent via mobile phone to Mazumdar-Shaw – believed to be the largest cancer center in the world – and the Beckman Laser Institute for assessment.
The study is in its first phase. Teams from Beckman and Mazumdar-Shaw have traveled India gauging mobile phone reception, and a prototype of the device has been tested on a small group of patients. Wilder-Smith and Kuriakose say these early-stage efforts are promising, and they’re gearing up for a larger cohort of subjects across the vast nation.
“We’re in the process of reviewing the data now to figure out where we draw the lines that determine whether a measurement signifies that the tissues are normal or precancerous or malignant,” Wilder-Smith says. “We’re really satisfied with the progress.”
She’s already on to the next breakthrough. With a collaborator at the University of Arizona, she’s creating a snap-on laser device for smartphones that can also perform lesion analysis in the field. The technology – which would let field-workers easily send test data to a faraway cancer center – is in its experimental phase, and the researchers are seeking funding to support further development.
“We are truly advancing methods to remotely use laser technology to diagnose tissues, which can help out both patients and oncologists,” says Wilder-Smith, proving once again that she’s finding a better way.