Revving up research
Year-old center for accelerating clinical trials gave UCI Health an investigative edge when the pandemic hit
Back in mid-March, when COVID-19 became a worldwide crisis, UCI Health clinicians were poised to quickly begin working on possible treatments to tame the deadly virus.
The prior summer, after three years of planning, the UCI Center for Clinical Research had opened. It heralded a new era in UCI Health’s efforts to expand access to breakthrough therapies by accelerating clinical trials – research studies seeking ways to prevent, detect and treat diseases.
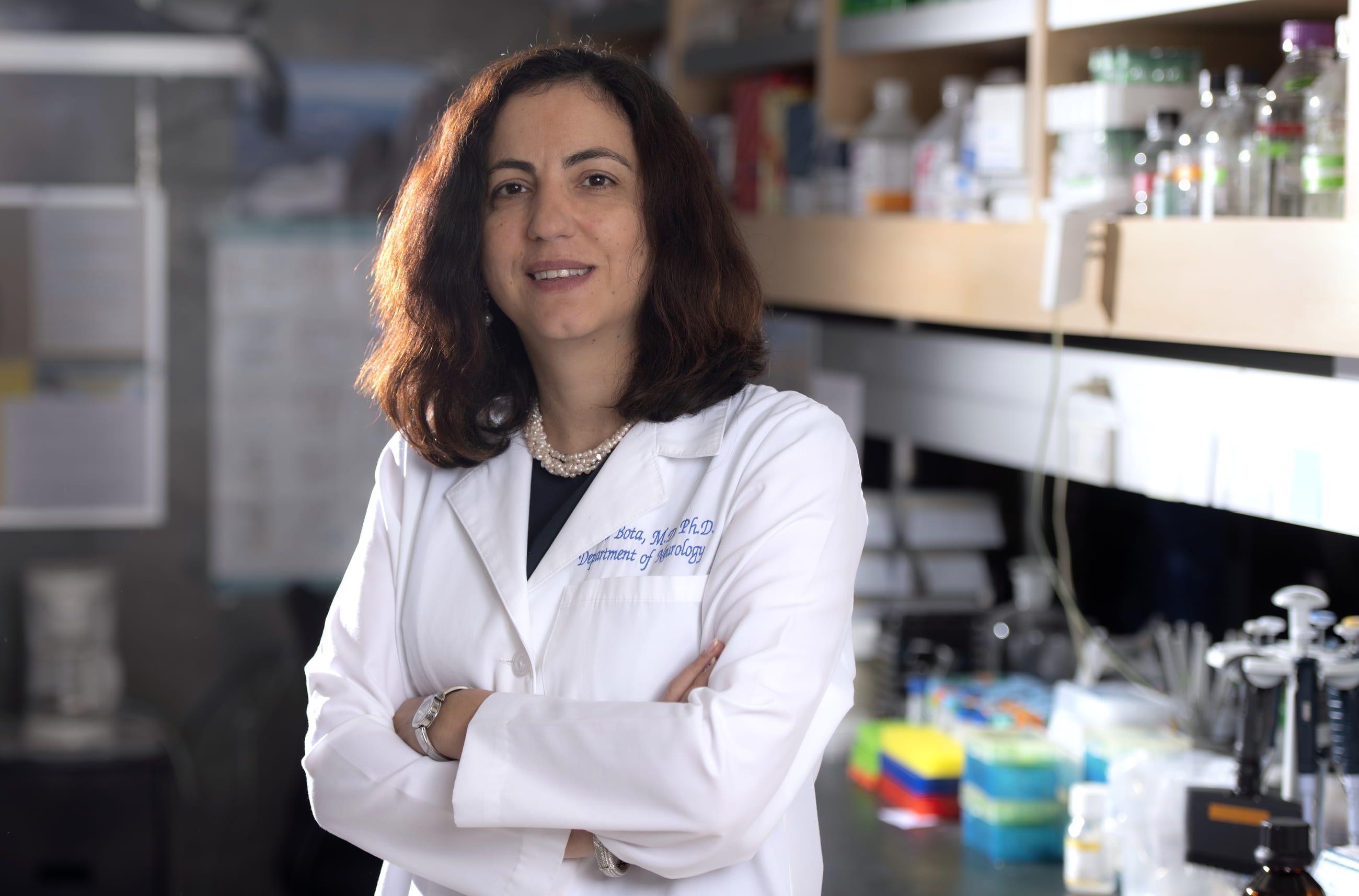
“This [launch] was extremely timely,” says Dr. Daniela Bota, vice dean of clinical research and medical director of the center, which now has 75 principle investigators and 120 clinical researchers on staff. “When COVID-19 hit, we had some advantages.”
By May 1, six weeks after the coronavirus was declared a global pandemic, UCI Health had become one of the first designated sites in the country to start conducting research into the utility of remdesivir – an investigational, broad-spectrum antiviral medication – as a potential therapy for COVID-19.
A short time after that, on May 19, UCI Health began its second coronavirus clinical trial, this one to determine how effective aviptadil is in critically ill patients suffering from acute respiratory distress syndrome. The drug has a 20-year history of safe use in humans for lung ailments.
Since then, UCI Health has initiated four more clinical trials to fight different aspects of the disease caused by SARS-CoV-2, Bota says. One involves developing an inhaler to keep patients off ventilators. Another examines ways to prevent UCI Health workers from getting sick. Yet another study is assessing the efficacy of convalescent plasma – plasma from people who have recovered from COVID-19 – injected into ailing individuals.
“And there are more [coronavirus] clinical trials on the way,” says Bota, adding that nondisclosure agreements do not permit her to elaborate. But in one, she says, a local company is working to come up with a vaccine.
Most clinical trials at research hospitals, she says, can take up to nine months to launch. But because of the groundwork established by UCI Health with the opening of the Center for Clinical Research, that time has been slashed to three months or less.
“The idea was for us to facilitate clinical trials,” says Bota, a neuro-oncologist who made a name for herself with groundbreaking research on glioblastoma, the most aggressive form of brain cancer. “At other universities, they’ll have one study here, one study there, but no central office and no ability to accelerate the process.”
By the onset of the pandemic, the Center for Clinical Research had remedied that at UCI Health. “We had this structure, and we had established relations with the majority of big pharmaceutical companies,” Bota says. “Second, we had a single point of contact. And third, we had a well-oiled system in which studies were already staffed and defined.”
All noncancer clinical trials at UCI Health go through the center and involve multiple physicians with different clinical interests. For example, the principal investigators on the remdesivir trial are Dr. Alpesh N. Amin (chair of medicine, hospitalist) and Dr. Lanny Hsieh (infectious diseases), while Dr. Richard Lee (pulmonary and critical care) heads up the aviptadil trial.
Dr. Donald Forthal (infectious diseases) and Dr. Minh-Ha Tran (transfusion medicine, pathology) are leading the clinical trial of convalescent plasma. The substance is seen as a possible treatment for COVID-19 until a vaccine is developed, Bota says.
It confers “passive immunity,” she notes, and can shorten the amount of time a critically ill COVID-19 patient has to be on a ventilator. Convalescent plasma is also eligible for compassionate use in patients who don’t meet certain criteria to participate in clinical trials.
Although the pandemic has put a focus on COVID-19 research, UCI Health boasts an impressive depth and breadth of studies.
The UCI Center for Clinical Research currently oversees some 300 industry-funded interventional clinical trials – those with patients receiving experimental treatments. These trials are underway in 12 departments, including dermatology, urology, neurology and obstetrics-gynecology. And there are an equal number of research studies in progress that do not yet involve patients.
“Our portfolio is very wide,” Bota says. “Much of our work lies in developing novel, cutting-edge cellular and genetic engineering therapies for life-threatening diseases.”
She’s quick to credit a critical component of clinical trials: the people who opt to join them.
“Many patients come to UCI because of our clinical trials,” Bota says. “They are extremely generous and want to participate in them. Many have publicly said how much potential hope we’re bringing everybody because they have direct access to what we offer.”