Blood will tell
UCI researchers create coronavirus microarray test to determine true prevalence of COVID-19 infection and gauge antibody responses
Just a little pinprick.
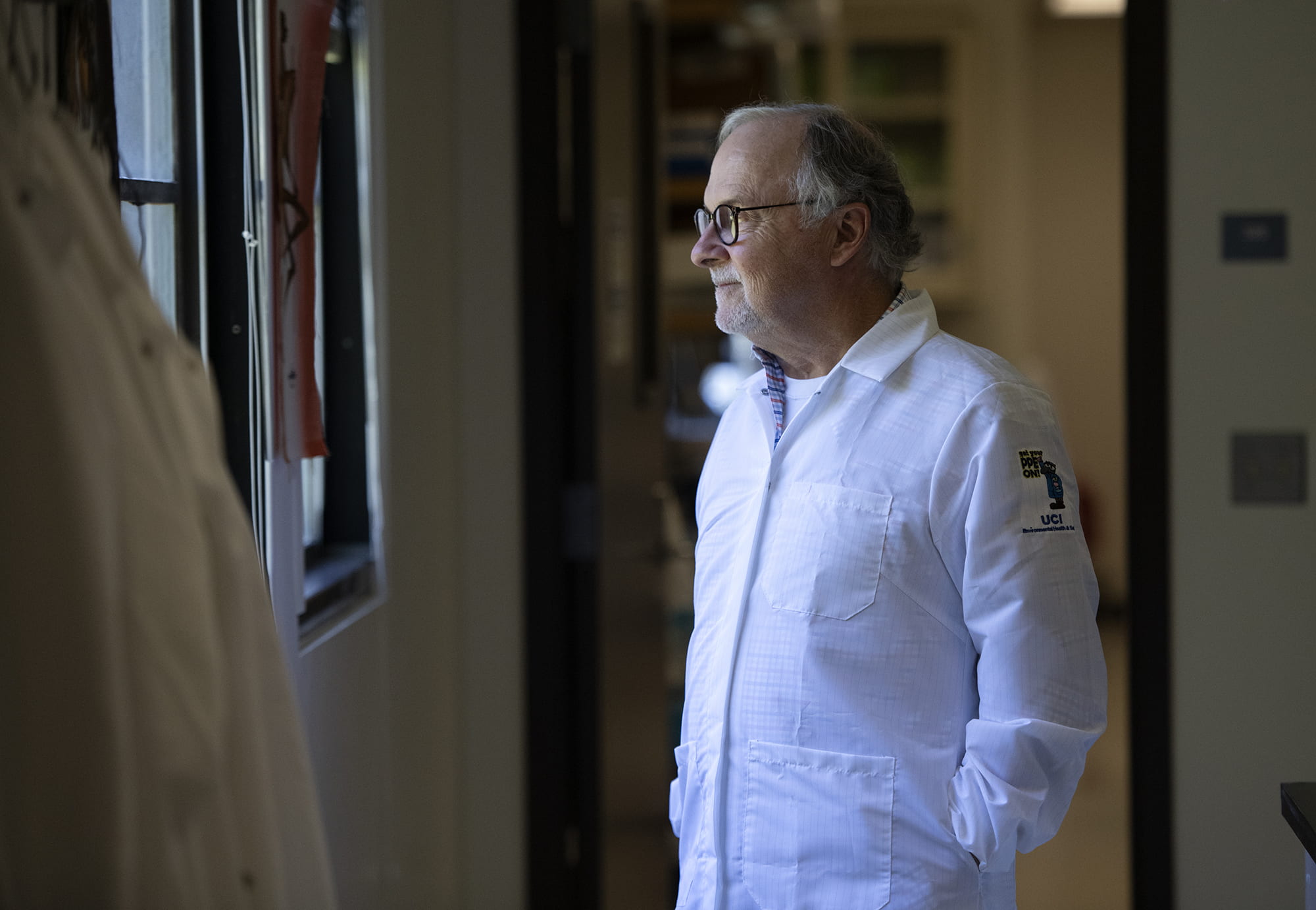
For Phil Felgner, director of the Vaccine R&D Center in the UCI School of Medicine’s Institute for Immunology, that’s the key to learning more about how humans respond to the COVID-19 virus, as well as to gaining more insight into a possible vaccine and to understanding how social distancing and other protective measures are working.
Beginning the week of May 18, Felgner and researchers in his lab began taking blood samples from UCI Medical Center employees who consented to having their fingers jabbed to see if they’ve been exposed to COVID-19.
“People want this kind of test,” he says, adding that it’s crucial in determining how widespread SARS-CoV-2 is in the population.
The familiar nasal swabs, which enable standard polymerase chain reaction testing, provide far less accurate information about COVID-19 immunity, Felgner says. Plus, he notes, most individuals getting them already show symptoms of COVID-19 – while a lot of those infected are either asymptomatic or only mildly affected.
The nasal swab tests look for genetic evidence of the coronavirus. PCR technology involves greatly amplifying this material, if it’s present. But this method underestimates the true prevalence of COVID-19 infection, says Felgner, adjunct professor of physiology & biophysics.
Comparing to other diseases
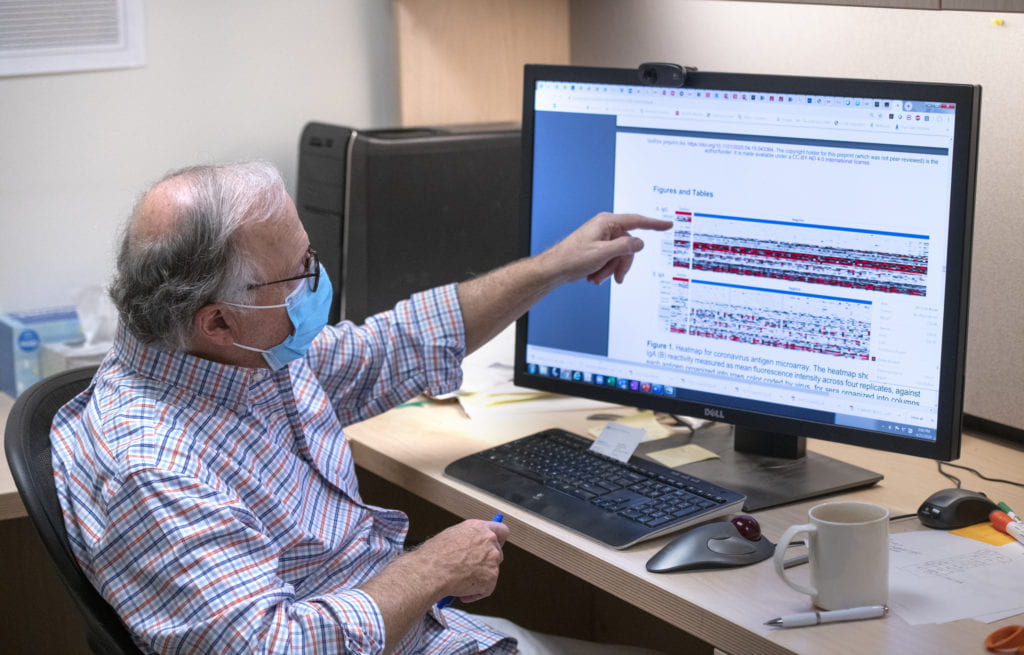
His team has developed a coronavirus antigen microarray – a collection of microscopic DNA bits affixed to a solid surface, such as a glass slide – that holds hundreds of different types of disease proteins, such as those from influenza, malaria, common human coronaviruses, other respiratory viruses and now COVID-19.
Blood samples are compared to each of these disease proteins to determine a person’s antibody response – and help researchers understand why some people get seriously ill with COVID-19 while others don’t.
The antigen microarray, dubbed COVAM, can also be used to shed light on additional mysteries about SARS-CoV-2 infection, including whether baseline serology for other coronaviruses influences the course of COVID-19, how an individual’s antibody response to infection evolves over time, and what antigens would be optimal for vaccine development.
Over the next several weeks, Felgner and his lab members plan to collect samples from 1,000 UCI Medical Center employees and 5,000 Orange County residents who don’t work there to seek answers to the most critical questions that researchers, as well as the general public, are asking:
- Were the flu-like symptoms I just experienced from COVID-19?
- Do I have antibodies against SARS-CoV-2, the virus that causes COVID-19?
- Do my antibodies against SARS-CoV-2 protect me from COVID-19?
- Do I need to get sick to generate antibodies that protect me from COVID-19, or is an asymptomatic infection enough?
- How can I tell when I have an asymptomatic exposure that induces protective antibodies against SARS-CoV-2?
- How long will my protective antibodies last?
- Are we building up herd immunity worldwide over time against the SARS-CoV-2 virus?
- Will the herd immunity we develop this year last until next year?
“We have to get these answers,” says Felgner, who has been at UCI since 2002. “My parents were children during the 1918 Spanish flu outbreak. It feels as if we’re having an experience like that now.”
Feeling useful
Felgner says he’s never been busier in his professional life, “but I feel useful.” His email has more than tripled, with many messages from colleagues in the scientific community asking about his research and possible collaborations. Many more are from people wanting their blood tested for COVID-19.
“We feel privileged that we’re in a position to really contribute so much to solving this problem,” Felgner says, speaking for his team.
Prior to the pandemic, they were trying to produce a vaccine for Q fever, a bacterial infection that humans typically get by inhaling dust contaminated by infected animals. They also were working on an influenza vaccine.
Felgner has applied for a provisional patent on COVAM because of technologies developed by his lab. And the group is consulting with UCI Beall Applied Innovation’s research translation group. In addition, Felgner has partnered with a company in China that has good proteins for the microarray. So far, this collaboration has resulted in the creation of 15,000 tests to distribute worldwide.
Previously, microarray tests have been used to detect antibodies against certain strains of SARS and MERS, Felgner says. Now they’re being used to learn more about COVID-19 and conquer the disease.
“The way the scientific infrastructure has been able to converge on this pandemic – and how our funding agencies have focused so much attention on it so quickly – should give everybody a lot of optimism about the future,” he says.