Fending off the flu
UCI expert discusses facts and fallacies about seasonal scourge and staying healthy through the holidays

The holiday season kicks off on Thanksgiving. And while feasts with family and friends are among the highlights, such gatherings also hasten exposure to the flu, which strikes up to 20 percent of U.S. residents each year. More than 200,000 are hospitalized annually for influenza-related complications.
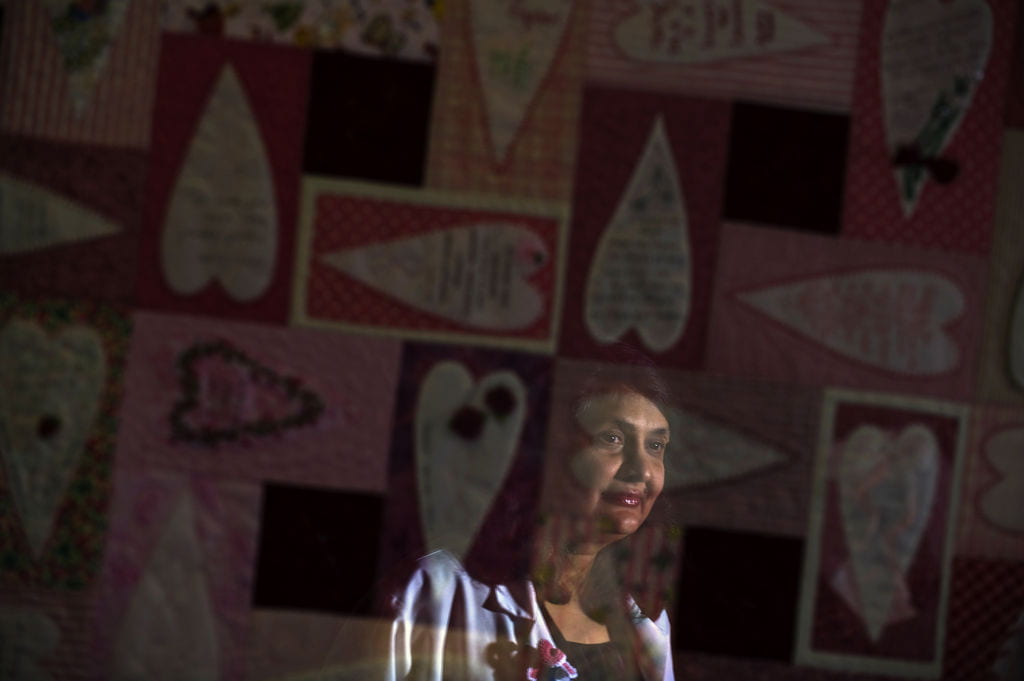
Andrew Noymer, UC Irvine associate professor of public health and an expert on flu pandemics, encourages vaccination and frequent hand-washing to ward off illness. Here, he discusses this recurrent scourge and ways to protect the most vulnerable among us.
Q. Can we make any predictions about the severity of the 2013-14 flu season? What type of influenza virus is circulating right now?
A. At this time, it’s too early to say how severe or mild the flu season will be. It really gets going in December and peaks in the new year. There are no new human-to-human pandemic strains, although the H7N9 avian virus in Asia is being monitored closely. Pandemic strains can emerge at any time, even outside the traditional flu season. For example, the most recent H1N1 pandemic began in April 2009. Currently, there are H1N1 and H3N2 strains in circulation.
Q. What are the benefits of early vaccination?
A. The flu vaccine doesn’t take effect for a few days and can require up to 10 days to reach full protection. So waiting until the middle of the flu season may not be as effective as getting a flu shot early.
Q. Sometimes people who get the flu vaccine still get sick. Why is this so?
A. There are two reasons for this – and one big misconception. The first reason is that there are thousands of cold viruses, and in any given locale in any given winter, a dozen or more of these may be in circulation. The flu vaccine protects against the flu virus, not against other viruses that cause flu-like illness. It’s commonplace to say that one “has the flu” when, in reality, it’s a bad cold. The second reason is that the flu vaccine is not 100 percent effective. The misconception is that the flu vaccine works by creating a small illness that generates antibodies that protect against later illness. People who feel ill after a flu shot often assume the vaccination caused it. But flu shots contain no live virus and do not work that way. Some vaccines do work that way – for example, the Sabin polio vaccine (but not the Salk polio vaccine). Getting an influenza shot is no guarantee you won’t get a coincidental cold, but it does not cause a mild case of flu. There is one exception: FluMist, administered as a nasal spray, is a live, attenuated virus vaccine and can cause a short and extremely mild coldlike syndrome.
Q. How many people usually die from the flu each year? Who’s at risk?
A. There are about 36,000 influenza deaths annually in the U.S. (This is an estimate, since the number of laboratory-confirmed influenza deaths is much lower.) Most occur among those 65 and older. Infants are also among the most vulnerable.
Q. What made the 1918 flu pandemic so deadly? Do innovations in modern medicine and public health policy ensure that we won’t see another such flu season?
A. The 1918 pandemic was the result of the emergence of a very novel (at the time) H1N1 strain of influenza. There are different theories as to why it was so deadly, all of which involve the virus’s novelty. In contrast, the most recent pandemic – in 2009 – was rather mild, and this is because the virus strain was not as dissimilar to those recently in circulation. Our ability to respond to a pandemic is much stronger now than in 1918, and overall disease prevention is much better, reducing the chance of polymicrobial infections, which contributed to mortality in 1918. However, there’s no guarantee that another highly virulent strain of influenza won’t emerge. The 1918 pandemic killed 0.5 percent of the U.S. population, so even something half as deadly could kill more than 750,000 people today.
Q. What can people do to stay healthy?
A. The Centers for Disease Control & Prevention recommends vaccination for everyone over 6 months old. In addition, frequent hand-washing with soap (and/or the use of alcohol-based hand sanitizer) is encouraged. The flu virus can live for up to four hours on surfaces such as doorknobs, and it can infect us if we touch a contaminated surface and then touch our eyes, nose or mouth. Since studies have shown that people often touch their face unconsciously, the best defense is frequent hand-washing. It’s also important to stay home from work or school if one has respiratory symptoms or a fever. This prevents spreading it to others.
Q. How important is it for the population to be properly vaccinated against the flu? Do high vaccination rates result in lower mortality rates?
A. Vaccination has been shown to be effective against the flu, which is why the CDC recommends it. Whether vaccination reduces mortality is a complex question and the subject of debate among flu researchers. Most people who die of influenza are elderly, and because the immune system naturally wanes with age, the vaccine may be less effective among the elderly. Thus, the impact of vaccination may be greater in preventing sickness among adults and children than in preventing deaths among the elderly – but we’re not sure. It’s an active area of research. It’s especially important not to visit a place like a nursing home if one is sick with the flu, since outcomes such as death are more common among the elderly.
Q. What’s the relationship between the flu and pneumonia?
A. Pneumonia is an infection and inflammation of the lungs that can arise as a complication of influenza. There are other germs that can cause pneumonia – the bacterium pneumococcus (Streptococcus pneumoniae), for example – so not all pneumonia is caused by the flu virus. However, pneumonia is a frequent severe complication of the flu, especially among the elderly. When someone dies from a case of influenza, it’s really from pneumonia. Fever and difficulty breathing are symptoms, and anyone showing these signs should get to a doctor immediately.
Q. Any other messages to the public?
A. People should not panic, but they can and should methodically protect themselves and others by: vaccination; hand-washing or sanitizing; covering the mouth and nose when coughing or sneezing; staying home from work or school when sick; and avoiding visits to nursing homes when any flu symptoms are present.